Prepare to Meet the Future with Data
We revisit ONC’s Information Blocking Rule, recap public comments, and look at how health plans can meet data sharing requirements.
Earlier this year, we wrote about the ONC’s proposed information blocking rule and how it serves as an opportunity for health plans. The proposed rule faced a public comment period (which closed last month) during which major industry concerns were voiced. The consensus by many seems to be that ONC’s rule lacks clarification in key areas while inadvertently increasing complexity (and cost) in others.
But as they say, “the writing’s on the wall” for health data interoperability and broader access to electronic health information. Where does this leave health plans? A recent study by Deloitte predicts that healthcare organizations are standing at the precipice of innovation. But first, let’s look at the feedback that the proposed information blocking rule received.
Industry Response to the Information Blocking Rule
One thing we can agree on at this point: interoperability is a major objective for our industry. But those who would be affected by the Information Blocking Rule have asked the ONC to revise or even revoke the current rule. This includes the Federal Trade Commission, who despite being consulted on the proposed rule, issued a letter asking the ONC to consider refinements. Notably, eHealth Initiative (eHI) offered the following comments and concerns:
Scope of “Electronic Health Information” is too broad, should be defined
Conditions and Maintenance of Certification (APIs)
Too complex and costly as proposed
Too much risk to providers and patients, specifically the proposed “Click Yes to Continue” model does not adequately portray data security risk to patient
Information Blocking
Healthcare actors should be defined in the final rule
Complex and costly documentation requirements
Greater Data Sharing is the Goal
The ONC has stated that greater interoperability is the goal of the proposed Information Blocking Rule. Improved data sharing is a worthy objective for health plans because it’s an easy effort to prove value on. Health plans have a competitive edge over their counterparts when they are more integrated with providers and members. In addition to priming plans to be compliant with whatever final rule is based, improving access to data is also key to readying for other initiatives, such as alternative payment models.
Of course, we know that total healthcare data interoperability sounds like the answer to all your challenges. But once the hard work begins of solving this problem, it can feel like data sharing at the level required is next to impossible. We’re here to tell you it’s not; interoperability is a realistic goal with the right technology.
We know that our industry is on the precipice of innovation. The recent study from Deloitte referenced above and in our prior article posits healthcare is on the precipice of a “20 to 30 year industry transformation. The industry forces and the disruption that’s upon us are true indicators that we’re going to be going through a cycle of innovation.” Innovation made possible by radical data interoperability.
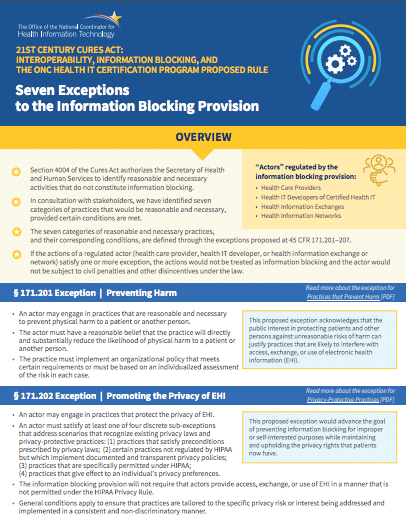
ONC’s Information Blocking Rule has 7 exceptions. Do you know what they are?
See the official list here.
The Promise of Big Data
Improved access to data is considered a consumer-driven shift, one often compared to the Amazon experience where a consumer can have on-demand access to personal information. But getting personalized, real-time electronic health data at the click of a button is a lot more complicated than it sounds. And it requires a special relationship that has historically been difficult: high-level collaboration between payers and providers.
Yet this demand is exactly the kind of opportunity health plans can seize upon as they search out competitive ways to utilize big data. Examples can be seen in the use of predictive analytics to mitigate risk, noted in this article as a “massive moneysaver” by one health plan who made a big IT investment. Reams of data are available to health plans — all that’s lacking is the right way to connect and analyze it.
“Improving relationships with members and providers is already a focus for health plans, and data sharing is another way to accomplish that goal.”
Health plan of the future? It starts with data sharing.
One way of looking at the Information Blocking Rule is that it’s a proposed answer to a problem that health plans can take control of now. Improving data sharing isn’t just a proactive approach to anticipated regulation — it’s becoming an essential business function for health plans. To get started, health plans can focus on these three areas:
Develop data analytics and predictive modeling know-how
Take advantage of opportunities to break down data silos by fostering relationships with providers, members and vendors
Look for existing technology that can support these goals: bring disparate data together, simplify data modeling, and provide a transparent communications platform
The future of data sharing is now. Pareo® is how.
Now’s the time for total payment integrity
See the ClarisHealth 360-degree solution for total payment integrity in action.

